John C Licciardone,1Matthew J Schultz,1 and Brook Amen2
Abstract
Chronic pain is a common condition that often interferes with work or other activities. Guidelines support the use of non-pharmacological treatments, such as spinal manipulation, in patients with chronic pain. Osteopathic physicians in the United States are uniquely positioned to manage chronic pain because their professional philosophy embraces the biopsychosocial model and they are trained in the use of osteopathic manipulative treatment (OMT) to complement conventional medical care. This narrative review provides current perspectives on the osteopathic approach to chronic pain management, including evidence for the efficacy of OMT based on systematic searches of the biomedical literature and the ClinicalTrials.gov database. Men, persons with low levels of education, and non-White and Hispanic patients are significantly less likely to have received OMT during their lifetime. Patients with low back and neck pain are most likely to be treated with OMT, and osteopathic manipulative medicine specialty physicians and family medicine physicians most often use OMT. However, many osteopathic physicians report using OMT infrequently. Although OMT is considered safe, based on millions of patient encounters over more than a century, there is limited evidence on its efficacy in treating chronic pain. The lone exception involves chronic low back pain, wherein there is evidence from systematic reviews, a large clinical trial, and observational studies. There is lesser evidence to support cost effectiveness and patient satisfaction associated with OMT for chronic pain. The only clinical practice guideline established by the American Osteopathic Association recommends that OMT should be used to treat chronic low back pain in patients with somatic dysfunction. Given the philosophy of osteopathic medicine, universal training of osteopathic physicians to use OMT, and national guidelines supporting non-pharmacological treatments for chronic pain, it is unclear why OMT use is reported to be remarkably low in physician surveys.Keywords: osteopathic manipulative treatment, chronic pain, somatic dysfunction, randomized controlled trial, cost effectiveness, patient satisfactionGo to:
Chronic Pain in the United States
The Institute of Medicine report on Relieving Pain in America in 2011 declared that chronic pain is a biopsychosocial condition that often requires integrated, multimodal, and interdisciplinary treatment, all components of which should be evidence-based.1 The National Pain Strategy2 and the Federal Pain Research Strategy3 subsequently developed coordinated approaches aimed at reducing the burden of pain in the United States. These clinical and research efforts both must be informed by and responsive to the biopsychosocial mechanisms that produce and maintain chronic pain, thereby leading to the development of safe and effective pain treatments.2 The Centers for Disease Control and Prevention (CDC) issued guidelines in 2016 for prescribing opioids for chronic pain.4 These guidelines recommended non-pharmacological treatment as an initial preferred approach for chronic pain management. The American College of Physicians subsequently issued a clinical practice guideline in 2017 that similarly recommended nonpharmacological treatment, including spinal manipulation, as the initial approach to patients with chronic low back pain.5 Despite such efforts and guidance over the past decade, the CDC recently estimated that 50 million adults in the United States suffer from chronic pain, including 20 million with high-impact chronic pain that interferes with work or life most days or every day.6 This narrative review provides current perspectives on the osteopathic approach to the management of chronic pain in the United States, including evidence for the efficacy of osteopathic manipulative treatment (OMT) based on systematic searches of the biomedical literature and the ClinicalTrials.gov database.Go to:
Historical Overview of Osteopathic Medicine
Osteopathy was founded in the United States in 1874 by Andrew Taylor Still, a frontier doctor in the Midwest. Still embraced two major elements within his new system of healing. These comprised the restoration of bodily structure and function through palpatory assessment and manipulative treatment, and a holistic view that included physical, mental, and spiritual health. The American School of Osteopathy was eventually established in Kirksville, Missouri in 1892. As schools of osteopathy evolved over the ensuing decades they became colleges of osteopathic medicine that accepted into their curricula the scientific advances that facilitated the development of new diagnostic technologies and the improved safety and effectiveness of drug therapies. Consequently, a convergence of osteopathic and allopathic medicine occurred in the latter half of the 20th century, with remarkable growth in the numbers of colleges of osteopathic medicine and osteopathic physicians that continues to this day. Nevertheless, such growth and convergence with allopathic medicine has led some to question the fundamental role of osteopathic principles and practice, particularly palpatory diagnosis and OMT, within the osteopathic profession in the 21st century.7Go to:
Osteopathic Principles and Practice
The four key principles of osteopathic philosophy are: the human body is a dynamic unit of function; the body possesses self-regulatory mechanisms that are healing in nature; structure and function are interrelated at all levels; and rational treatment is based on these principles.8 The “holistic” approach that is often attributed to osteopathic medical care is based upon these principles, which preceded the now widely accepted biopsychosocial model. A host of social factors that contribute to chronic pain are considered and addressed during the delivery of medical care under either paradigm.9 Thus, osteopathic physicians are uniquely positioned to manage patients with chronic pain because their philosophy embraces a biopsychosocial approach to patient care.10,11
Contemporary thought includes five models that may explain the osteopathic approach to patient care: biomechanical, respiratory-circulatory, metabolic-energy, neurological, and behavioral.8 As espoused in the biomechanical model, osteopathic palpatory diagnosis and OMT are used to alleviate somatic dysfunction and thereby restore normal motion and function throughout the body. In the behavioral model, a holistic approach involves physical, psychological, social, cultural, behavioral, and spiritual aspects of medical care so that a collaborative patient-physician relationship may be established. The biomechanical and behavioral models are most highly relevant to the osteopathic approach to chronic pain management when viewed within the biopsychosocial paradigm. It is worth noting that the primary aims of the osteopathic approach are to restore function and promote health-related quality of life, not necessarily to reduce pain intensity. Thus, the osteopathic approach is congruent with recent views that a primary focus on pain intensity is misguided in the management of patients with chronic pain.12,13
Preliminary research found that osteopathic physicians indeed displayed a practice style that was consistent with osteopathic principles, and that was most evident during patient encounters involving low back pain.14 More recent research provides further evidence that osteopathic physicians are more highly rated on measures of interpersonal manner and empathy than allopathic physicians, and that osteopathic medical care is associated with better clinical outcomes in patients with chronic low back pain.15 Most recently, it has been shown that patients treated by osteopathic physicians who use OMT for chronic low back pain report lesser pain intensity and back-related disability, while less often using opioids and nonsteroidal anti-inflammatory drugs, than patients treated by allopathic physicians.16 The latter study also found that the outcomes of patients treated by osteopathic physicians who did not use OMT were comparable to those of patients treated by allopathic physicians, and were significantly worse than those of patients treated by osteopathic physicians who used OMT for chronic low back pain.Go to:
Osteopathic Manipulative Treatment and Techniques
Somatic dysfunction is defined as impaired or altered function of related components of the body framework system: skeletal, arthrodial, and myofascial structures, and their related vascular, lymphatic, and neural elements.17 Somatic dysfunction is characterized by positional asymmetry, restricted range of motion, tissue texture abnormalities, or tenderness.17 The latter may include pain elicited through palpation. Osteopathic manipulative treatment is used to alleviate somatic dysfunction by applying manually guided forces to improve physiologic function and support homeostasis.17 Research indicates that OMT is most often used to treat restricted range of motion and least often to treat tenderness or pain.18 These findings coincide with the biomechanical model of osteopathic medical practice and align with efforts to reduce pain impact rather than merely focusing on pain intensity.6,12,13
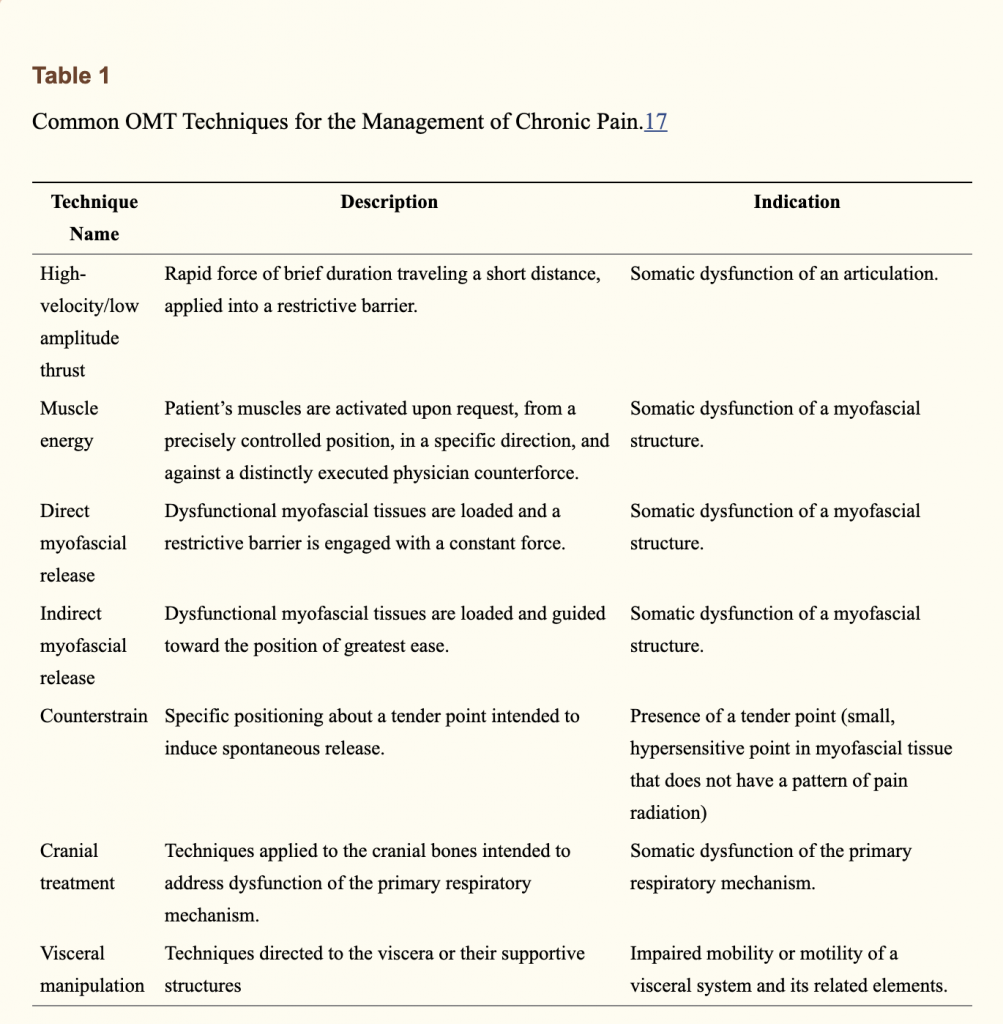
Osteopathic manipulative treatment consists of more than 100 different techniques.19 The OMT techniques commonly used to treat chronic pain are summarized in Table 1. The use of these techniques varies according to such factors as the somatic dysfunction to be treated and the training and proficiency of the osteopathic physician. A majority of patients treated with OMT have musculoskeletal complaints, although there is extensive involvement of other body systems.20 Consequently, osteopathic manipulative medicine (OMM) specialists and family medicine physicians are most likely to use OMT. Whereas OMM specialists are more likely to use fascial ligamentous release techniques and cranial techniques, family medicine physicians more often report using high-velocity, low-amplitude thrusts than non-primary care physicians.21
The selection of an OMT technique should be based on the etiology of the somatic dysfunction, patient characteristics and preferences, and physician level of proficiency with different techniques.22 The etiologies of somatic dysfunction often interact through biomechanics and neurological reflexes. For example, positional asymmetry of an articular structure may shorten one muscle group while lengthening the antagonist muscle group, resulting in myofascial tissue texture changes. Thus, an articular somatic dysfunction may produce a secondary myofascial somatic dysfunction. In this case, patient response and physician judgment will determine whether one or more OMT techniques are needed to address the resultant physical findings and restore homeostasis.
Patient characteristics and preferences should be considered when selecting an appropriate OMT technique.22 Special consideration should be given to patient age and comorbid conditions. For example, more forceful techniques (eg, high-velocity, low-amplitude thrusts) should be avoided in older patients and in those with osteoporosis to prevent the risk of injury. Likewise, infants and young children are generally unable to adequately respond to verbal instruction, thereby precluding techniques (eg, muscle energy techniques) that require active patient participation. However, patients with prior exposure to OMT may have meaningful input regarding positive or negative responses to certain treatment techniques in the past. Eliciting such information when selecting OMT techniques allows physicians to actively engage patients in their treatment plan and promotes shared decision-making.
Because the effectiveness of OMT depends upon its skilled application, physicians should consider their level of proficiency when selecting among potentially indicated techniques. It is unlikely that osteopathic physicians will be equally and highly proficient in all of the many techniques, particularly if they are not trained as OMM specialists or infrequently use OMT. Thus, physicians should select techniques they are comfortable performing. The potential risk with a given OMT technique should be balanced with the aforementioned patient and physician factors prior to its selection. Gentle techniques are generally preferred over more forceful techniques to minimize the risk of injury.Go to:
Evidence for the Efficacy of Osteopathic Manipulative Treatment of Chronic Pain
Two systematic searches of the biomedical literature were performed to find relevant studies of OMT for chronic pain. The first search, which was performed in January 2020 and focused on individual studies, identified 239 citations (Supplemental Appendix 1). The second search, which was performed in February 2020 and focused on related systematic reviews and meta-analyses, identified 49 citations (Supplemental Appendix 2). A final search of the ClinicalTrials.gov database was performed in March 2020 using the term “osteopathic” filtered for studies that were “interventional,” “completed,” and “with results.” Of the 18 studies identified in this search, only the results for the OSTEOPATHIC Trial were relevant to this review (Supplemental Appendix 3).
These individual studies and systematic reviews primarily involved OMT in the management of chronic low back pain. The earliest review, which conducted meta-analysis of six trials that included a total of 525 patients, concluded that OMT significantly reduced low back pain intensity.23 The reported effect size for OMT in reducing pain intensity (Cohen’s d=0.30) is consistent with a small treatment effect, based on recommendations established by the Cochrane Back Review Group (Cohen’s d<0.5).24 Nevertheless, this OMT effect size is comparable to that reported for nonsteroidal anti-inflammatory drugs.25 The studies included in this review did not provide sufficient data to conduct meta-analysis of physical functioning or quality-of-life outcomes. Although the use of osteopathy in Europe and other nations is beyond the scope of this review because of heterogeneous regulatory statues and practice rights around the globe, it is noteworthy that the magnitude of OMT effects was comparable in the three trials conducted in the United States (Cohen’s d=0.31) as compared with the three trials in the United Kingdom (Cohen’s d=0.29).23 There was not a sufficient number of trials to conduct meta-analyses according to the chronicity of low back pain. However, a subgroup analysis involving four trials with long-term follow-up extending up to 1 year (ie, suggesting relevance to chronic low back pain) found significant reductions in low back pain intensity with OMT (Cohen’s d=0.41). Based largely on the results of this review, the American Osteopathic Association developed and issued its first clinical practice guideline in 2010.26 The guideline provided an algorithm for decision making pertaining to the use of OMT in patients with low back pain and supports the use of OMT in patients with chronic low back pain, as manifested by somatic dysfunction.
A subsequent review, which conducted meta-analysis of 10 trials that included a total of 1141 patients, similarly concluded that OMT significantly reduced low back pain intensity.27 However, a majority of the trials included in the meta-analyses for all low back pain (and specifically for chronic low back pain) were conducted outside the United States. The reported overall effect size for OMT in reducing pain intensity (weighted mean difference=12.91) represents a medium treatment effect (weighted mean difference, 10–20).24 The larger number of trials and patients in this review enabled meta-analyses of functional status. A significant improvement in functional status was observed with OMT (standardized mean difference=0.36), which represents a small treatment effect (standardized mean difference<0.5).24 Meta analyses that included only trials of patients with chronic low back pain similarly found significant results for pain intensity (weighted mean difference=14.93; medium treatment effect) and functional status (standardized mean difference=0.32; small treatment effect). Although these systematic review findings were included in the updated American Osteopathic Association clinical practice guideline for low back pain, the treatment algorithm and recommendations for OMT use remained unchanged.28
The OSTEOPATHIC Trial is the largest randomized controlled trial conducted to assess the efficacy of OMT for chronic low back pain.29 It consisted of a 2 x 2 factorial design, wherein 455 patients were randomized to OMT, ultrasound therapy, or their respective sham comparators. The OMT group received six treatments over 8 weeks based on an algorithmic approach that targeted the lumbosacral, iliac, and pubic regions to receive high-velocity, low-amplitude thrusts; moderate-velocity, moderate-amplitude thrusts; soft tissue stretching, kneading, and pressure; myofascial stretching and release; counterstrain treatment; and muscle energy techniques. Intention-to-treat analyses conducted at 12 weeks post-randomization found significant reductions in pain intensity with OMT, all in the range of medium treatment effects29 (risk ratios for moderate and substantial pain improvements ranging from 1.25 to 2.0).24 Although significant improvements in back-related functioning or general health were not observed in patients in the OMT group, they reported significantly lesser use of prescription medication for low back pain during the trial.
Subsequent analyses of the OSTEOPATHIC Trial data were performed based on new recommendations for reporting study outcomes that emerged from the National Institutes of Health Task Force on Research Standards for Chronic Low Back Pain.30 These analyses, the results of which were published after the American Osteopathic Association updated its clinical practice guideline, focused on responder analysis for chronic pain recovery31 and cumulative distribution functions for treatment response.32 Recovery from chronic low back pain at the 12-week end point was defined using the rigorous composite measure of pain intensity ≤10 mm/100mm on a visual analogue scale and disability score ≤2/24 on the Roland-Morris Disability Questionnaire for back-related functioning.33 A significantly increased likelihood of recovery from chronic low back pain was observed in the OMT group (risk ratio=2.36).31 This met the criterion for a large treatment effect (risk ratio>2),24 and the effect persisted after adjustment for potential confounders. Cumulative distribution functions also found large treatment effects with OMT in the subgroups of patients with baseline pain intensity scores ≥35 mm/100mm on a visual analogue scale and with baseline Roland-Morris Disability Questionnaire scores ≥16/24.32 It was recommended that patients with chronic low back pain having such levels of pain intensity or back-related disability be targeted to receive a trial of OMT prior to using more costly or invasive treatments.
There exists only a limited amount of evidence for the efficacy of OMT in chronic pain conditions other than low back pain. A systematic review of OMT for chronic neck pain included three trials with a total of 123 patients.34 The related meta-analysis found significant improvement in pain intensity representing a medium treatment effect (weighted mean difference=13.04), but without significantly improved functional status. The study findings were limited by small sample size, heterogeneity of comparator groups, and lack of long-term followup.
Another systematic review of OMT for headache included five trials with a total of 265 patients.35 Three trials investigated tension-type headache and the other two studied migraine headache. These studies generally demonstrated that OMT decreased pain intensity and frequency, decreased medication use, or improved quality-of-life in patients with tension-type or migraine headache. However, meta-analysis was not performed because of the heterogeneity of studies, which were also noted to be of relatively poor quality.Go to:
Safety of Osteopathic Manipulative Treatment of Chronic Pain
Osteopathic manipulative treatment is generally considered to be safe, particularly when performed by physicians trained in the United States. Historically, most reports of serious adverse events potentially associated with OMT have been based on anecdotal evidence or sporadic case reports. A major review of reported injuries following manipulative therapies included 128 articles published from 1925 to 1993 in 15 countries.36 The review found 115 reported injuries in the United States during this time period. However, osteopathic physicians were implicated in only two of these injuries. The remaining injuries were presumably attributed to other types of manipulative therapy practitioners, allied health professionals, or lay persons. The limitations of such research are that only serious injuries are likely to be reported and that the actual number of persons at risk of injury is generally unknown. Nevertheless, the review estimated that several hundred million manipulative treatments were performed annually in the United States at the time.
The cervical region is among the most likely to be injured or adversely affected by the use of spinal manipulation to manage pain. Although arterial dissections or aneurysms have been reported following such manipulation, studies of these phenomena have been largely limited to chiropractic manipulation.37–39 Such cases have been rarely, if ever, reported among patients treated by osteopathic physicians in the United States.36 The rarity of such serious adverse events renders impractical the use of prospective cohort studies to assess incidence rates and risk factors, and even retrospective case-control studies have not been conducted. Unlike with chronic low back pain, there have been no major trials of OMT for neck pain to prospectively assess the risk of common or serious adverse events.
Adverse events were reported by 6% of patients with chronic low back pain randomized to OMT in the OSTEOPATHIC Trial, which involved receiving six treatments over a period of 8 weeks.29 This incidence of adverse events was not significantly different than that reported in the sham OMT group. The incidence of adverse events following OMT has been more generally assessed in an osteopathic practice-based research network in the United States.40 Therein, an adverse event incidence rate of 2.5% was observed immediately after OMT among 925 patients who participated in 1915 office encounters. However, no comparator group was available for study. The most commonly reported adverse event was pain or discomfort. Remarkably, it was reported that high-velocity, low-amplitude thrusts were significantly less likely to be associated with adverse events immediately after treatment than were other OMT techniques (odds ratio=0.22). The prevention of adverse events may be enhanced by using patient risk stratification to determine the appropriateness of OMT in various pain management scenarios.41Go to:
Cost Effectiveness of Osteopathic Manipulative Treatment of Chronic Pain
Few studies have addressed the cost effectiveness of OMT for chronic pain conditions in the United States. Systematic reviews of the cost effectiveness of OMT in a broader context have highlighted many of the limitations of the studies published in this area.42,43 Nevertheless, the Medical Expenditure Panel Survey was used to compare the cost effectiveness of six medical specialties and four other health care professionals in treating back and joint problems.44 The medical specialty described as “osteopathic medicine” likely represented physicians who routinely used OMT in their practice (ie, OMM specialists). The study found that these osteopathic medicine physicians were cost effective in achieving combined physical and mental health outcomes in the patient domains of mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. However, the study did not provide results that were specific to patients with chronic pain.Go to:
Patient Satisfaction with Osteopathic Manipulative Treatment of Chronic Pain
Somewhat more research has been conducted on patient satisfaction with OMT for chronic pain. A study of patients seen at an OMM specialty clinic that primarily treated musculoskeletal conditions, including chronic low back pain, found that patients were most satisfied with the interpersonal manner of their physicians.45 In that study, overall patient satisfaction was highly associated with perceived efficacy of OMT and improvement in pain or discomfort with OMT. An early randomized controlled trial of OMT for chronic low back pain found that patients who received OMT were significantly more likely to report global satisfaction with their back care over a period of 6 months than patients who received no intervention.46 Subsequently, the OSTEOPATHIC Trial found that patients who received OMT were significantly more likely to report being very satisfied with their back care over a period of 12 weeks than patients who received sham OMT.29 Registry patients with chronic low back pain who received care from osteopathic physicians have also reported higher levels of satisfaction with physician interpersonal manner than patients treated by allopathic physicians, while also reporting lesser back-related disability.15Go to:
Challenges in Implementing Osteopathic Manipulative Treatment of Chronic Pain
The extent to which OMT is used in medical practice is highly variable despite the required training received by all osteopathic physicians in the United States.47–50 The Osteopathic Survey of Health Care in America found that men, persons with low levels of education, and non-White and Hispanic patients were significantly less likely to have ever received OMT during their lifetime.51
These findings suggest that perceptional and economic barriers may exist in accessing OMT. Results from the National Ambulatory Medical Care Survey demonstrate that osteopathic physicians treat a disproportionately large percentage of patients with low back and neck pain;52 however, the specific use of OMT in such patients cannot be measured with the available data. Further results from the latter study indicate that the amount of time spent by osteopathic physicians in treating patients during primary care visits for low back pain (17.9 min) and neck pain (17.3 min) is not significantly different than the time spent by allopathic physicians in treating such patients with low back pain (17.9 min) and neck pain (18.6 min).52 These findings suggest that osteopathic physicians infrequently spend time to deliver OMT in addition to other services required during medical encounters for chronic pain within the context of a busy primary care setting. Correspondingly, a majority of osteopathic physicians in a national survey reported that they used OMT on less than 5% of their patients, although virtually all of them agreed that it is an efficacious treatment.47 Similarly, in a survey of osteopathic physicians practicing in Ohio, almost one-half of respondents reported that they had not used OMT on any patient during the previous week.49
Factors consistently associated with decreased OMT use in medical practice include lacking satisfactory OMT training in the postdoctoral years, practicing in a non-primary care specialty, and being unprepared to integrate OMT into practice.47–49 These inhibitory factors are likely to intensify as more osteopathic medical students seek training in residency programs under the umbrella of the Accreditation Council for Graduate Medical Education and proportionately fewer graduates enter primary care specialties (particularly family medicine) wherein OMT is more likely to be used. Under such circumstances, it is difficult to envision OMT remaining as an integral aspect of the professional identity of osteopathic medicine.53 Interestingly, lack of conclusive evidence of the efficacy of OMT (other than for low back pain) is infrequently cited by osteopathic physicians as a reason for not using it in medical practice. Conversely, there has not been any evidence to show that development and dissemination of the American Osteopathic Association guidelines26,28 have increased the use of OMT in patients with chronic low back pain.Go to:
Challenges in Performing Research on Osteopathic Manipulative Treatment of Chronic Pain
There are unique challenges in performing research on the efficacy and safety of OMT for chronic pain, particularly clinical trials.54 The prevailing standards in designing clinical trials have been largely developed in response to the need for assessing new drugs for specific indications. These usually involve rigid research protocols within the context of explanatory trials to assess efficacy. Such trials of OMT are difficult to perform. Fundamentally, the use of OMT should be guided by palpatory examination for somatic dysfunction. However, osteopathic physicians demonstrate substantial variability in their diagnosis of somatic dysfunction and, consequently, their approach to OMT.18,21 Thus, unlike prescription drugs manufactured under strict quality control standards, OMT is an intervention that is inherently variable from one treatment session to another. Beyond inter-physician variability in diagnosis and treatment of somatic dysfunction, there is variability in the latter also attributable to patients. Chronic pain generally requires ongoing OMT that is tailored to the individual patient and that should be delivered through an iterative process that assesses somatic dysfunction and then responds with appropriate treatment. Other factors that warrant consideration within a clinical trial of OMT for chronic pain are the frequency and timing of treatment sessions, treatment fidelity among providers and over time, selection of appropriate control treatments, maintenance of OMT effect, and potential resolution of somatic dysfunction or recovery from chronic pain. For these reasons, pragmatic trials that assess the effectiveness of OMT for chronic pain and observational studies are generally more feasible than explanatory trials that assess OMT efficacy.Go to:
Conclusions
Osteopathic physicians in the United States are uniquely positioned to manage chronic pain because their professional philosophy embraces the biopsychosocial model and they are trained in the use of OMT to complement conventional medical care. Nevertheless, national surveys indicate that men, persons with low levels of education, and non-White and Hispanic patients are significantly less likely to have ever received OMT in their lifetime, and that many osteopathic physicians infrequently use OMT in medical practice. Osteopathic manipulative treatment is most often used by patients with low back and neck pain. Although OMT is considered safe, based on millions of patient encounters over more than a century, there is generally limited evidence on its efficacy for chronic pain. However, there is substantial evidence from systematic reviews, a large clinical trial, and observational studies to support its use in patients with chronic low back pain. Consequently, the only clinical practice guideline established by the American Osteopathic Association supports the use of OMT to treat chronic low back pain in patients with somatic dysfunction. Given this and other national guidelines relating to non-pharmacological treatments for chronic pain, it is unclear why osteopathic physicians do not report using OMT more often.Go to:
Disclosure
The authors report no conflicts of interest in this work.Go to:
References
1. Institute of Medicine. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington, DC: The National Academies Press; 2011. [Google Scholar]
2. Interagency Pain Research Coordinating Committee. National pain strategy: a comprehensive population health-level strategy for pain. National Institutes of Health; 2016. Available from: https://www.iprcc.nih.gov/sites/default/files/HHSNational_Pain_Strategy_508C.pdf. Accessed April10, 2020.
3. Interagency Pain Research Coordinating Committee. Federal Pain Research Strategy. National Institutes of Health; 2017. Available from: https://iprcc.nih.gov/sites/default/files/FPRS_Research_Recommendations_Final_508C.pdf. Accessed April10, 2020.
4. Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain — United States, 2016. MMWR Recomm Rep. 2016;65(No. RR–1):1–49. doi:10.15585/mmwr.rr6501e1 [PubMed] [CrossRef] [Google Scholar]
5. Qaseem A, Wilt TJ, McLean RM, Forciea MA; Clinical Guidelines Committee of the American College of Physicians. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2017;166(7):514–530. doi:10.7326/M16-2367 [PubMed] [CrossRef] [Google Scholar]
6. Dahlhamer J, Lucas J, Zelaya C, et al. Prevalence of chronic pain and high-impact chronic pain among adults – United States, 2016. MMWR Morb Mortal Wkly Rep. 2018;67(36):1001–1006. doi:10.15585/mmwr.mm6736a2 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
7. Gevitz N. Center or periphery? The future of osteopathic principles and practices. J Am Osteopath Assoc. 2006;106(3):121–129. [PubMed] [Google Scholar]
8. Seffinger MA, Hruby RJ, Rogers FJ, et al. Philosophy of osteopathic medicine In: Seffinger MA, Hruby R, Willard FH, Licciardone J, editors. Foundations of Osteopathic Medicine: Philosophy, Science, Clinical Applications, and Research. 4th ed. Philadelphia, PA: Wolters Kluwer; 2018:2–18. [Google Scholar]
9. Gatchel RJ. Comorbidity of chronic pain and mental health disorders: the biopsychosocial perspective. Am Psychol. 2004;59(8):795–805. doi:10.1037/0003-066X.59.8.795 [PubMed] [CrossRef] [Google Scholar]
10. Licciardone JC. The unique role of osteopathic physicians in treating patients with low back pain. J Am Osteopath Assoc. 2004;104(11 Suppl 8):S13–S18. [PubMed] [Google Scholar]
11. Minotti D, Licciardone JC, Kearns C, Gatchel RJ. Osteopathic medicine: approach to pain management. Pract Pain Manag. 2010;28–29, 32–34, 37–38. [Google Scholar]
12. Ballantyne JC, Sullivan MD. Intensity of chronic pain–the wrong metric? New Engl J Med. 2015;373(22):2098–2099. doi:10.1056/NEJMp1507136 [PubMed] [CrossRef] [Google Scholar]
13. Sullivan MD, Ballantyne JC. Must we reduce pain intensity to treat chronic pain? Pain. 2016;157(1):65–69. doi:10.1097/j.pain.0000000000000336 [PubMed] [CrossRef] [Google Scholar]
14. Carey TS, Motyka TM, Garrett JM, Keller RB. Do osteopathic physicians differ in patient interaction from allopathic physicians? An empirically derived approach. J Am Osteopath Assoc. 2003;103(7):313–318. [PubMed] [Google Scholar]
15. Licciardone JC, Schmitt ME, Aryal S. Osteopathic and allopathic physician interpersonal manner, empathy, and communication style and clinical status of their patients: a pain registry-based study. J Am Osteopath Assoc. 2019;119(8):499–510. doi:10.7556/jaoa.2019.092 [PubMed] [CrossRef] [Google Scholar]
16. Licciardone JC, Gatchel RJ. Osteopathic medical care with and without osteopathic manipulative treatment in patients with chronic low back pain: a pain registry-based study. J Am Osteopath Assoc. 2020;120(2):64–73. doi:10.7556/jaoa.2020.016 [PubMed] [CrossRef] [Google Scholar]
17. Educational Council on Osteopathic Principles. Glossary of osteopathic terminology In: Seffinger MA, Hruby R, Willard FH, Licciardone J, editors. Foundations of Osteopathic Medicine: Philosophy, Science, Clinical Applications, and Research. 4th ed. Philadelphia, PA: Wolters Kluwer; 2018:1563–1594. [Google Scholar]
18. Licciardone JC, Kearns CM, King HH, et al. Somatic dysfunction and use of osteopathic manual treatment techniques during ambulatory medical care visits: a CONCORD-PBRN study. J Am Osteopath Assoc. 2014;114(5):344–354. doi:10.7556/jaoa.2014.072 [PubMed] [CrossRef] [Google Scholar]
19. Lesho EP. An overview of osteopathic medicine. Arch Fam Med. 1999;8:477–484. doi:10.1001/archfami.8.6.477 [PubMed] [CrossRef] [Google Scholar]
20. Johnson SM, Kurtz ME. Conditions and diagnoses for which osteopathic primary care physicians and specialists use osteopathic manipulative treatment. J Am Osteopath Assoc. 2002;102(10):527–532, 537–540. [PubMed] [Google Scholar]
21. Johnson SM, Kurtz ME. Osteopathic manipulative treatment techniques preferred by contemporary osteopathic physicians. J Am Osteopath Assoc. 2003;103(5):219–224. [PubMed] [Google Scholar]
22. Hruby RJ. The osteopathic manipulative treatment prescription In: Seffinger MA, Hruby R, Willard FH, Licciardone J, editors. Foundations of Osteopathic Medicine: Philosophy, Science, Clinical Applications, and Research. 4th ed. Philadelphia, PA: Wolters Kluwer; 2018:784786. [Google Scholar]
23. Licciardone JC, Brimhall AK, King LN. Osteopathic manipulative treatment for low back pain: a systematic review and meta-analysis of randomized controlled trials. BMC Musculoskel Disord. 2005;6:43. doi:10.1186/1471-2474-6-43 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
24. Furlan AD, Pennick V, Bombardier C, van Tulder M. 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine. 2009;34(18):1929–1941. doi:10.1097/BRS.0b013e3181b1c99f [PubMed] [CrossRef] [Google Scholar]
25. Bjordal JM, Ljunggren AE, Klovning A, Slordal L. Non-steroidal anti-inflammatory drugs, including cyclo-oxygenase-2 inhibitors, in osteoarthritic knee pain: meta-analysis of randomised placebo controlled trials. BMJ. 2004;329(7478):1317. doi:10.1136/bmj.38273.626655.63 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
26. Clinical Guideline Subcommittee on Low Back Pain. American Osteopathic Association guidelines for osteopathic manipulative treatment (OMT) for patients with low back pain. J Am Osteopath Assoc. 2010;110(11):653–666. [PubMed] [Google Scholar]
27. Franke H, Franke JD, Fryer G. Osteopathic manipulative treatment for nonspecific low back pain: a systematic review and meta-analysis. BMC Musculoskel Disord. 2014;15:286. doi:10.1186/1471-2474-15-286 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
28. Task Force on the Low Back Pain Clinical Practice Guidelines. American Osteopathic Association guidelines for osteopathic manipulative treatment (OMT) for patients with low back pain. J Am Osteopath Assoc. 2016;116(8):536–549. doi:10.7556/jaoa.2016.107 [PubMed] [CrossRef] [Google Scholar]
29. Licciardone JC, Minotti DE, Gatchel RJ, Kearns CM, Singh KP. Osteopathic manual treatment and ultrasound therapy for chronic low back pain: a randomized controlled trial. Ann Fam Med. 2013;11(2):122–129. doi:10.1370/afm.1468 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
30. Deyo RA, Dworkin SF, Amtmann D, et al. Report of the NIH Task Force on Research Standards for Chronic Low Back Pain. J Pain. 2014;15(6):569–585. doi:10.1016/j.jpain.2014.03.005 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
31. Licciardone JC, Gatchel RJ, Aryal S. Recovery from chronic low back pain after osteopathic manipulative treatment: a randomized controlled trial. J Am Osteopath Assoc. 2016;116(3):144–155. doi:10.7556/jaoa.2016.031 [PubMed] [CrossRef] [Google Scholar]
32. Licciardone JC, Gatchel RJ, Aryal S. Targeting patient subgroups with chronic low back pain for osteopathic manipulative treatment: responder analyses from a randomized controlled trial. J Am Osteopath Assoc. 2016;116(3):156–168. doi:10.7556/jaoa.2016.032 [PubMed] [CrossRef] [Google Scholar]
33. Roland M, Morris R. A study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low-back pain. Spine. 1983;8(2):141–144. doi:10.1097/00007632-198303000-00004 [PubMed] [CrossRef] [Google Scholar]
34. Franke H, Franke JD, Fryer G. Osteopathic manipulative treatment for chronic nonspecific neck pain: a systematic review and meta-analysis. Int J Osteopath Med. 2015;18(4):255267. doi:10.1016/j.ijosm.2015.05.003 [CrossRef] [Google Scholar]
35. Cerritelli F, Lacorte E, Ruffini N, Vanacore N. Osteopathy for primary headache patients: a systematic review. J Pain Res. 2017;10:601–611. doi:10.2147/JPR.S130501 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
36. Vick DA, McKay C, Zengerle CR. The safety of manipulative treatment: review of the literature from 1925 to 1993. J Am Osteopath Assoc. 1996;96:113–115. doi:10.7556/jaoa.1996.96.2.113 [PubMed] [CrossRef] [Google Scholar]
37. Jones J, Jones C, Nugent K. Vertebral artery dissection after a chiropractor neck manipulation. Proc (Bayl Univ Med Cent). 2015;28(1):88–90. doi:10.1080/08998280.2015.11929202 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
38. Saeed AB, Shuaib A, Al-Sulaiti G, Emery D. Vertebral artery dissection: warning symptoms, clinical features and prognosis in 26 patients. Can J Neurol Sci. 2000;27(4):292–296. doi:10.1017/S0317167100001025 [PubMed] [CrossRef] [Google Scholar]
39. Albuquerque FC, Hu YC, Dashti SR, et al. Craniocervical arterial dissections as sequelae of chiropractic manipulation: patterns of injury and management. J Neurosurg. 2011;115(6):1197–1205. doi:10.3171/2011.8.JNS111212 [PubMed] [CrossRef] [Google Scholar]
40. Degenhardt BF, Johnson JC, Brooks WJ, Norman L. Characterizing adverse events reported immediately after osteopathic manipulative treatment. J Am Osteopath Assoc. 2018;118(3):141–149. doi:10.7556/jaoa.2018.033 [PubMed] [CrossRef] [Google Scholar]
41. Kuchera ML, Seffinger MA, Boesler D, Connett DA. Effectiveness and safety of osteopathic manipulative treatment In: Seffinger MA, Hruby R, Willard FH, Licciardone J, editors. Foundations of Osteopathic Medicine: Philosophy, Science, Clinical Applications, and Research. 4th ed. Philadelphia, PA: Wolters Kluwer; 2018:1531–1542. [Google Scholar]
42. Gamber R, Holland S, Russo DP, Cruser DA, Hilsenrath PE. Cost-effective osteopathic manipulative medicine: a literature review of cost-effectiveness analyses for osteopathic manipulative treatment. J Am Osteopath Assoc. 2005;105:357–367. [PubMed] [Google Scholar]
43. Steel A, Sundberg T, Reid R, et al. Osteopathic manipulative treatment: a systematic review and critical appraisal of comparative effectiveness and health economics research. Musculoskelet Sci Pract. 2017;27:165–175. doi:10.1016/j.math.2016.10.067 [PubMed] [CrossRef] [Google Scholar]
44. Wilson FA, Licciardone JC, Kearns CM, Akuoko M. Analysis of provider specialties in the treatment of patients with clinically diagnosed back and joint problems. J Eval Clin Pract. 2015;21(5):952–957. doi:10.1111/jep.12411 [PubMed] [CrossRef] [Google Scholar]
45. Licciardone J, Gamber R, Cardarelli K. Patient satisfaction and clinical outcomes associated with osteopathic manipulative treatment. J Am Osteopath Assoc. 2002;102(1):13–20. [PubMed] [Google Scholar]
46. Licciardone JC, Stoll ST, Fulda KG, et al. Osteopathic manipulative treatment for chronic low back pain: a randomized controlled trial. Spine. 2003;28(13):1355–1362. doi:10.1097/01.BRS.0000067110.61471.7D [PubMed] [CrossRef] [Google Scholar]
47. Johnson SM, Kurtz ME. Diminished use of osteopathic manipulative treatment and its impact on the uniqueness of the osteopathic profession. Acad Med. 2001;76(8):821–828. doi:10.1097/00001888-200108000-00016 [PubMed] [CrossRef] [Google Scholar]
48. Ray AM, Cohen JE, Buser BR. Osteopathic emergency physician training and use of osteopathic manipulative treatment. J Am Osteopath Assoc. 2004;104(1):15–21. [PubMed] [Google Scholar]
49. Spaeth DG, Pheley AM. Evaluation of osteopathic manipulative treatment training by practicing physicians in Ohio. J Am Osteopath Assoc. 2002;102(3):145–150. [PubMed] [Google Scholar]
50. Spaeth DG, Pheley AM. Use of osteopathic manipulative treatment by Ohio osteopathic physicians in various specialties. J Am Osteopath Assoc. 2003;103(1):16–26. [PubMed] [Google Scholar]
51. Licciardone JC. Awareness and use of osteopathic physicians in the United States: results of the Second Osteopathic Survey of Health Care in America (OSTEOSURV-II). J Am Osteopath Assoc. 2003;103(6):281–289. [PubMed] [Google Scholar]
52. Licciardone JC. A national study of primary care provided by osteopathic physicians. J Am Osteopath Assoc. 2015;115(12):704–713. doi:10.7556/jaoa.2015.145 [PubMed] [CrossRef] [Google Scholar]
53. Licciardone JC. Osteopathic research: elephants, enigmas, and evidence. Osteopath Med Prim Care. 2007;1:7. doi:10.1186/1750-4732-1-7 [PMC free article] [PubMed] [CrossRef] [Google Scholar]
54. Licciardone J. Research methods and evidence relating to osteopathic manipulative treatment In: Seffinger MA, Hruby R, Willard FH, Licciardone J, editors. Foundations of Osteopathic Medicine: Philosophy, Science, Clinical Applications, and Research. 4th ed. Philadelphia, PA: Wolters Kluwer; 2018:1518–1530. [Google Scholar]
Articles from Journal of Pain Research are provided here courtesy of Dove Press

